MAMMOGRAPHY

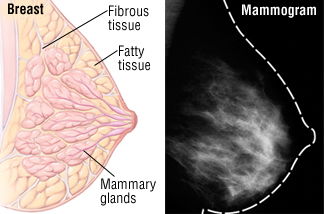
A mammogram is an x-ray picture of the breast. It can be used to check for breast cancer in women who have no signs or symptoms of the disease. It can also be used if you have a lump or other sign of breast cancer. Screening mammography is the type of mammogram that checks you when you have no symptoms.
Age before doing it:
Women ages 40 to 44 should have the choice to start annual breast cancer screening with mammograms (x-rays of the breast) if they wish to do so. Women age 45 to 54 should get mammograms every year. Women 55 and older should switch to mammograms every 2 years, or can continue yearly screening.
Screening tests are used to find cancer before a person has any symptoms. Here are the American Cancer Society's recommendations to help guide you when you talk to your doctor about screening for certain cancers.
Breast cancer
- Women ages 40 to 44 should have the choice to start annual breast cancer screening with mammograms (x-rays of the breast) if they wish to do so.
- Women age 45 to 54 should get mammograms every year.
- Women 55 and older should switch to mammograms every 2 years, or can continue yearly screening.
- Screening should continue as long as a woman is in good health and is expected to live 10 more years or longer.
- All women should be familiar with the known benefits, limitations, and potential harms linked to breast cancer screening.
Women should also know how their breasts normally look and feel and report any breast changes to a health care provider right away.
Some women – because of their family history, a genetic tendency, or certain other factors – should be screened with MRIs along with mammograms. (The number of women who fall into this category is very small.) Talk with a health care provider about your risk for breast cancer and the best screening plan for you.
Colon and rectal cancer and polyps
For people at average risk for colorectal cancer, the American Cancer Society recommends starting regular screening at age 45. This can be done either with a sensitive test that looks for signs of cancer in a person’s stool (a stool-based test), or with an exam that looks at the colon and rectum (a visual exam). Talk to your health care provider about which tests might be good options for you, and to your insurance provider about your coverage. No matter which test you choose, the most important thing is to get screened.
If you’re in good health, you should continue regular screening through age 75.
For people ages 76 through 85, talk with your health care provider about whether continuing to get screened is right for you. When deciding, take into account your own preferences, overall health, and past screening history.
People over 85 should no longer get colorectal cancer screening.
If you choose to be screened with a test other than colonoscopy, any abnormal test result needs to be followed up with a colonoscopy.
Cervical cancer
- Cervical cancer testing should start at age 21. Women under age 21 should not be tested.
- Women between the ages of 21 and 29 should have a Pap test done every 3 years. HPV testing should not be used in this age group unless it’s needed after an abnormal Pap test result.
- Women between the ages of 30 and 65 should have a Pap test plus an HPV test (called “co-testing”) done every 5 years. This is the preferred approach, but it’s OK to have a Pap test alone every 3 years.
- Women over age 65 who have had regular cervical cancer testing in the past 10 years with normal results should not be tested for cervical cancer. Once testing is stopped, it should not be started again. Women with a history of a serious cervical pre-cancer should continue to be tested for at least 20 years after that diagnosis, even if testing goes past age 65.
- A woman who has had her uterus and cervix removed (a total hysterectomy) for reasons not related to cervical cancer and who has no history of cervical cancer or serious pre-cancer should not be tested.
- All women who have been vaccinated against HPV should still follow the screening recommendations for their age groups.
Some women – because of their health history (HIV infection, organ transplant, DES exposure, etc.) – may need a different screening schedule for cervical cancer. Talk to a health care provider about your history.
Endometrial cancer
The American Cancer Society recommends that at the time of menopause, all women should be told about the risks and symptoms of endometrial cancer. Women should report any unexpected vaginal bleeding or spotting to their doctors.
Some women – because of their history – may need to consider having a yearly endometrial biopsy. Please talk with a health care provider about your history.Lung cancer
The American Cancer Society recommends yearly lung cancer screening with a low-dose CT scan (LDCT) for certain people at higher risk for lung cancer who meet the following conditions:
- Are aged 55 to 74 years and in fairly good health
and - Currently smoke or have quit smoking in the past 15 years
and - Have at least a 30 pack-year smoking history. (A pack-year is 1 pack of cigarettes per day per year. One pack per day for 30 years or 2 packs per day for 15 years would both be 30 pack-years.)
Before getting screened, you should talk to your health care provider about:
- Your risk for lung cancer
- How you can quit smoking, if you still smoke
- The possible benefits, limits, and harms of lung cancer screening
- Where you can get screened
You should also talk with your insurance provider about your coverage.
Prostate cancer
The American Cancer Society recommends that men make an informed decision with a health care provider about whether to be tested for prostate cancer. Research has not yet proven that the potential benefits of testing outweigh the harms of testing and treatment. We believe that men should not be tested without first learning about what we know and don’t know about the risks and possible benefits of testing and treatment.Starting at age 50, men should talk to a health care provider about the pros and cons of testing so they can decide if testing is the right choice for them.
If you are African American or have a father or brother who had prostate cancer before age 65, you should have this talk with a health care provider starting at age 45.
If you decide to be tested, you should get a PSA blood test with or without a rectal exam. How often you’re tested will depend on your PSA level.
Take control of your health, and help reduce your cancer risk.
Stay away from all forms of tobacco.- Get to and stay at a healthy weight.
- Get moving with regular physical activity.
- Eat healthy with plenty of fruits and vegetables.
- Limit how much alcohol you drink (if you drink at all).
- Protect your skin.
- Know yourself, your family history, and your risks.
- Get regular check-ups and cancer screening tests.
For more on what you can do to help reduce your cancer risk and other questions about cancer, please visit us online at www.cancer.org, or call us anytime, day or night, at +234-8038778988
